This week, we’re diving into an important and often challenging aspect of managing Postural Orthostatic Tachycardia Syndrome (POTS): physical activity. While increasing movement is widely recommended as part of non-pharmacologic therapy for POTS, it can be incredibly daunting for those experiencing severe symptoms like chronic pain and fatigue. Many traditional exercise programs fail to account for the complexity of POTS and its common comorbidities, leaving patients struggling to incorporate movement into their routines.
Join Dr. Linda Bluestein for a Webinar with Ehlers-Danlos Support UK
Hypermobility – Diagnosis and Treatment in the MCAS PatientSaturday, March 22, 2025 | 3:00 PM (UK time) | Online
Dr. Bluestein will discuss the diagnostic process for hEDS, key red flags, and factors contributing to persistent pain. She will also introduce her comprehensive treatment approach, the MENS PMMS method, for managing symptomatic joint hypermobility through movement, nutrition, sleep, psychosocial support, and more.
Register now to receive the webinar link and passcode.
Breaking Barriers: Rethinking Exercise and POTS
A recent peer-reviewed journal article, "Exercise in Postural Orthostatic Tachycardia Syndrome: Focus on Individualized Exercise Approach,” highlights a promising alternative: personalized, home-based exercise programs. Developed at the Dysautonomia Clinic, these tailored approaches are designed to be accessible and manageable, even for those who are home- or bedbound. By prioritizing patient education, pacing, and gradual progression, these programs help improve level of activity while minimizing the pitfalls of more rigorous, one-size-fits-all regimens.
Key Takeaways from the Article:
The Role of Deconditioning: Deconditioning is not the root cause of POTS, Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS), or orthostatic intolerance.
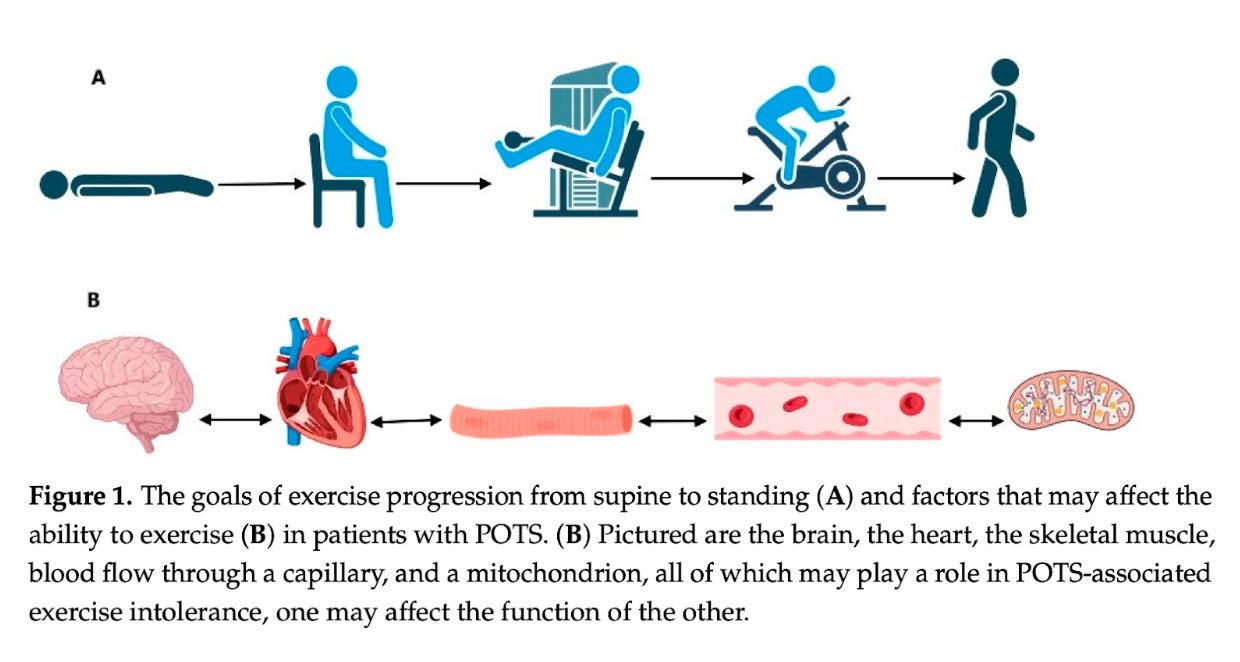
Exercise Intolerance is Multifactorial: Exercise intolerance in POTS is linked to several underlying mechanisms, such as reduced blood flow to the brain (cerebral hypoperfusion), impaired venous return, mitochondrial dysfunction affecting oxygen use, muscle abnormalities, and more.
Personalization is Critical: Individualized exercise plans focus on a patient’s unique symptoms, comorbidities, and physical limitations. This tailored approach maximizes benefits while minimizing risks like post-exertional malaise (PEM).
Remote Accessibility Matters: Home-based programs led by certified physical therapists provide a convenient and safe option for patients who cannot access outpatient facilities due to mobility, fatigue, or risk of infection.
Pacing and Gradual Progression: Starting with low-impact activities like reclining exercises, diaphragmatic breathing, and light core stabilization, many patients can gradually work toward standing activities and aerobic exercise such as swimming or cycling.
The Bigger Picture: Beyond symptom management, regular movement improves overall quality of life, mental health, and functional capacity, helping patients regain independence in daily activities.
Moving Forward
This innovative approach offers hope for patients with POTS, especially those with severe symptoms or additional conditions like ME/CFS or hypermobile Ehlers-Danlos Syndrome (hEDS). While more research is needed to refine and validate these methods, the Dysautonomia Clinic’s findings reinforce the importance of meeting patients where they are - both physically and emotionally.
Let’s continue to advocate for strategies that empower patients and respect the unique challenges they face! Movement is medicine - but only when it’s accessible, sustainable, and personalized.
For a deeper dive into the research and practical applications, check out the full article: Exercise in Postural Orthostatic Tachycardia Syndrome: Focus on Individualized Exercise Approach in the Journal of Clinical Medicine.
For more information, graphics, videos, and more follow Hypermobility MD on Instagram.
LAST THURSDAY: Solo Episode with Dr. Linda Bluestein
In this special solo episode of Bendy Bodies, I’m diving into the topics you wanted to hear more about—like hormone therapy, testosterone, and their impact on hypermobility. If you’ve been curious about these issues, don’t miss this deep dive into the latest science and practical strategies. Tune in now!
THIS THURSDAY: Dr. David Kaufman
In just a few days, I sit down with Dr. David Kaufman to uncover the most commonly overlooked factors in diagnosing and treating patients with hypermobility and other complex conditions. What are traditional approaches missing? And how can patients and practitioners work together to get the right answers? Don’t miss this essential conversation!
Well that’s all for this week; thank you so much for reading and supporting this newsletter. Talk to you soon, Bendy Buddies!
Yours in Health,
Dr. Bluestein