December’s final Bendy Bulletin is arriving a little early as we prepare for the holidays! While we’re stepping off our regular bi-monthly schedule, we’ll be back in January with even more insights to support the hypermobility community.
Today, we’re discussing an important topic: upper cervical instability (UCI) in hypermobile Ehlers-Danlos Syndrome (hEDS) and Hypermobility Spectrum Disorders (HSD). UCI is a complex and often debilitating complication that can impact neurological function and quality of life, but innovative neuroplasticity-based treatment approaches are opening new possibilities for care. Whether you’re a patient or a healthcare professional, this issue offers valuable information about safely managing UCI and improving outcomes.
This February 7-9, 2025 Hybrid Global Learning Conference is a great opportunity to collaborate, learn, and network. There are in-person interactive workshops that cover navigating healthcare systems, including funding access (NDIS), and managing cervical spine conditions.
This should not viewed as be an either-or. To be up to speed on all things EDS and HSD, you should attend this (all and Ehlers-Danlos Society Conferences) AND listen to all episodes of the Bendy Bodies podcast.
Managing Upper Cervical Instability in Hypermobility
While UCI has long been recognized for its joint-related complications, recent research highlights its complex neurological presentations and explores innovative conservative treatments rooted in neuroplasticity. Let’s dive in!
Why This Matters
UCI can significantly impact the brainstem, spinal cord, cranial nerves, and blood flow to the brain, leading to symptoms like dizziness, headaches, balance issues, and even pseudo-seizures. Traditional management has often relied on surgical fusion, which, while necessary in some cases, comes with high risks, costs, and variable outcomes. This week’s report focuses on a new, non-invasive neuroplasticity-based approach, offering hope for patients and clinicians alike.
What the Study Found
A recent brief report described three patients with severe UCI due to hEDS/HSD who were treated using a neuroplasticity-based physical therapy model. Each case highlighted the variability of outcomes in managing UCI conservatively:
Jay regained full function and returned to work with minimal flares after treatment.
Emma improved significantly but required surgical fusion due to severe symptoms and external challenges, including limited physical therapy access during COVID.
Kay faced ongoing severe neurological symptoms and frequent flares, achieving only modest improvements despite surgery and therapy.
These outcomes demonstrate the critical role of personalized care plans and the importance of addressing red flags (RFs) and yellow flags (YFs)—markers of neurological instability and stressors—that can impact prognosis.
A New Approach: Neuroplasticity in Physical Therapy
The neuroplasticity approach aims to retrain the nervous system and improve motor control through task-specific exercises and biofeedback. Key components include:
Posture and Alignment Training: Teaching patients to reduce strain during daily activities.
Proprioception and Motor Control Exercises: Gradually introducing controlled movements using biofeedback tools like laser alignment.
Functional Movement Training: Building stability and strength for daily activities.
This method carefully avoids interventions that could exacerbate symptoms, such as cervical mobilizations or high-intensity exercises, especially for patients with high-irritability UCI.
Insights from the Discussion
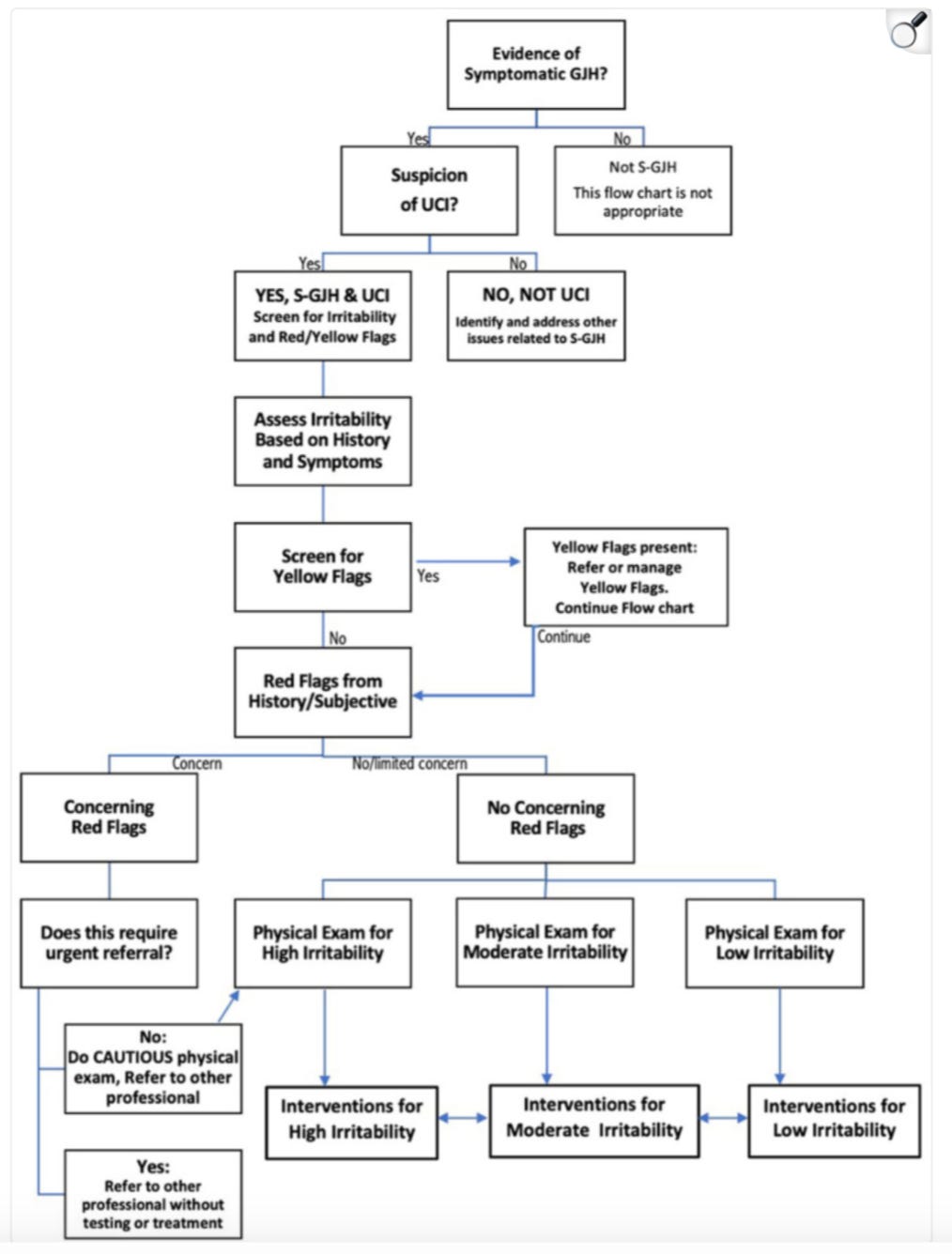
The study reinforces the importance of recent expert consensus guidelines for evaluating and managing UCI safely. Key takeaways include:
The Role of RFs and YFs: Patients with fewer RFs and better psychosocial support tend to have better outcomes. For example, Jay, with minimal RFs and strong family support, made a full recovery, while Kay, with numerous RFs and limited support, continued to struggle.
Complex Neurological Presentation: UCI often involves symptoms beyond joint instability, including cognitive changes, severe headaches, and balance issues. These complexities require careful screening and tailored interventions.
The Value of Neuroplasticity: Task-specific training and feedback-based exercises show promise in retraining the nervous system, improving motor control, and reducing disability.
While these findings are encouraging, the authors note that more research is needed to validate these treatment approaches and develop standardized guidelines.
What This Means for Patients and Providers
For patients: If you’re living with UCI, this study highlights the importance of seeking care from clinicians familiar with hypermobility-related disorders. A neuroplasticity-based physical therapy approach may offer a safer, less invasive alternative to surgery, particularly in milder cases.
For clinicians: This research provides a framework for safely assessing and treating UCI in hypermobile patients. By incorporating neuroplasticity principles and carefully monitoring RFs and YFs, you can help patients achieve better outcomes while minimizing risks.
Looking Ahead
This report serves as a pilot study for future research into conservative care for UCI. As understanding of neuroplasticity grows, it has the potential to revolutionize how we approach not only UCI but also other hypermobility-related disorders.
Together, let’s continue to explore these innovative treatments and share knowledge to improve care for the hypermobile community.
Presentation and physical therapy management using a neuroplasticity approach for patients with hypermobility-related upper cervical instability
Read the article that inspired this newsletter!
Upper cervical instability impacts many people with EDS and HSD.
Please check out these Bendy Bodies podcast episodes on cervical instability.
Episode 66 - CODIFYING UPPER CERVICAL INSTABILITY WITH LESLIE RUSSEK, DPT, PHD
Episode 75 - CERVICAL INSTABILITY: THINKING BEYOND THE NECK WITH PATTY STOTT, DPT
Episode 77 - NEUROSURGICAL INSIGHTS FROM PAOLO BOLOGNESE, MD AND GUEST COHOST PRADEEP CHOPRA, MD
THIS THURSDAY, December 19th: A Special Solo Episode with Dr. Linda Bluestein
This week, it’s just me, Dr. Linda Bluestein, and I’m excited to bring you a special solo episode! We’ll dive deep into some of the most pressing questions about hypermobility, Ehlers-Danlos Syndromes (EDS), and living well with these complex conditions. I also discuss how Anthem Blue Cross introduced time limits on anesthesia coverage, how MCAS management is personalized, food allergy testing limitations, and my Coaching vs. Medical Appointments.
NEXT THURSDAY, December 26th: Dr. Satish Raj
This week, we’re excited to welcome Dr. Satish Raj to the podcast, where he’ll share his expertise on the connection between hypermobility and dysautonomia, including conditions like POTS (Postural Orthostatic Tachycardia Syndrome). Dr. Raj’s groundbreaking research and clinical insights shed light on how these conditions intersect and what that means for diagnosis, management, and improving quality of life. This is a conversation you won’t want to miss!
Well that’s all for this week; thank you so much for reading and supporting this newsletter. Talk to you soon, Bendy Buddies!
Yours in Health,
Dr. Bluestein









Thank you for this. I had a Foramen Magnum meningioma removed 20 years ago. Suboccipial left craniotomy, posterior arch of C1 removed, and left laminectomy of C2. Professionals I’ve seen have remarked at the musculature of my neck, presumably in response to the disruption. Often I get pops and clunks with electrical shots to my arms and torso. We are survivors and warriors.
To Linda Bluestein, MD: Perhaps you would be interested in this: CVJinstability.org