Why Are Constipation and Diarrhea So Common in EDS?
Welcome back to The Bendy Bulletin!
Today we’re diving into a crucial topic for anyone with hypermobility: gut issues. Specifically, we’re exploring what gastroenterologists should know about hypermobile Ehlers–Danlos Syndrome and the often-overlooked connection between hEDS and gastrointestinal dysfunction. If you’ve ever felt like your stomach has a mind of its own, this one’s for you.
Want more? Become a paid subscriber to unlock extra newsletters, exclusive interviews, subscriber-only chats, and access to replays of my upcoming LIVE video Q&As and interviews. This community is growing - and you won’t want to miss what’s next.
I’m excited to invite you to a special event that could truly change the way you navigate your medical journey.
Ask an Independent Patient Advocate: The EDS Edition
🗓 Tuesday, September 10th at 5pm CT / 6pm ET
I’ll be joined by Maggie Buckley, instructor of the EDS ECHO Advocacy Program, to answer your questions about independent patient advocacy - what it is, how it helps, and why it matters for people with EDS, MCAS, and other complex chronic conditions.
Hosted by Greater National Advocates, this conversation is for anyone looking for real-world strategies and support from professionals who get it. Whether you're new to advocacy or already considering a partner in your care, this session will offer valuable insights.
Constipation. Diarrhea. Bloating. Nausea. Sound familiar?
If you’re living with hypermobile Ehlers-Danlos Syndrome (hEDS), a hypermobility spectrum disorder (HSD), or another connective tissue condition, you’ve probably had your fair share of gut trouble – and maybe even been told it’s all in your head.
It’s not.
In fact, gastrointestinal (GI) symptoms are among the most commonly reported – and least understood – aspects of these conditions.
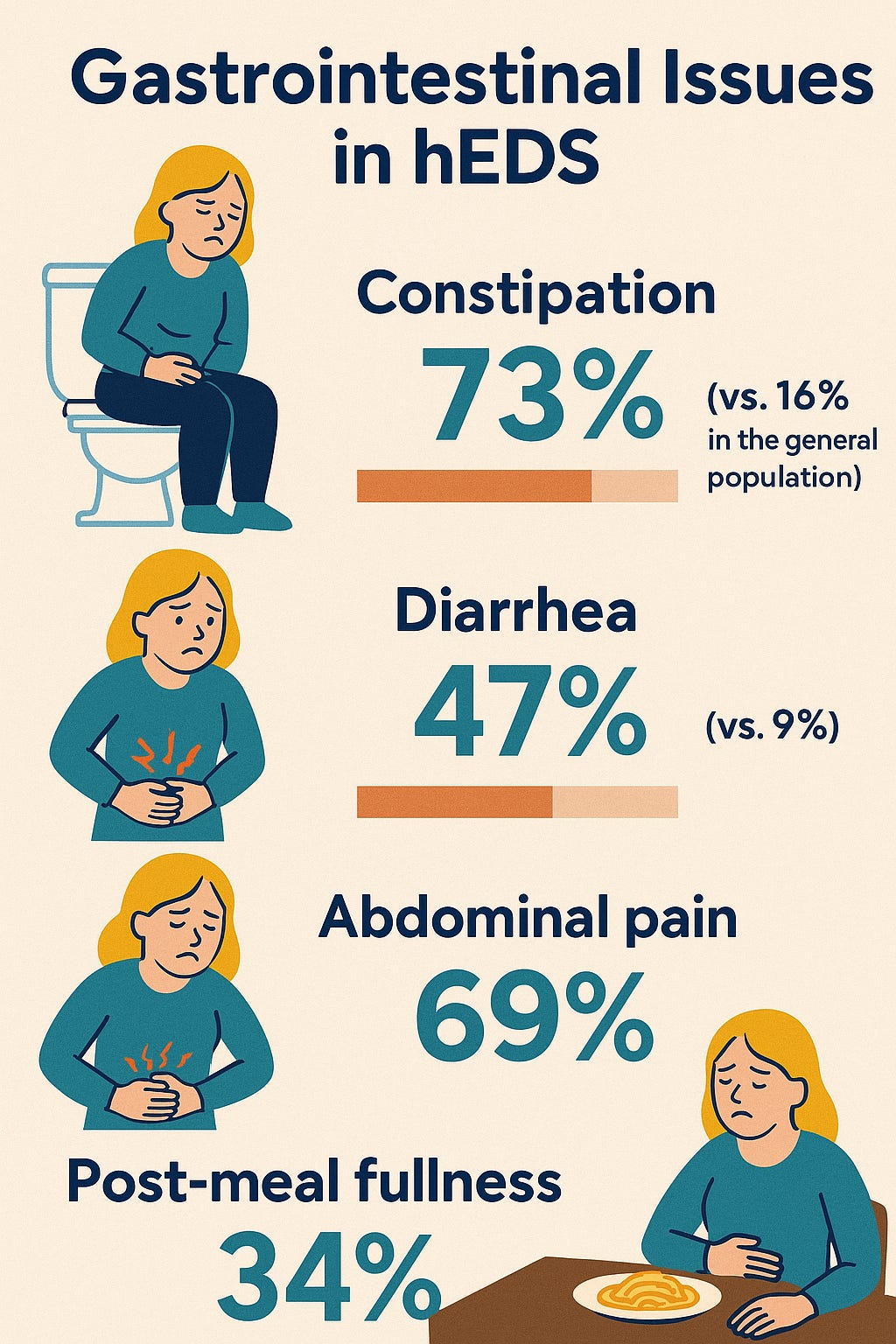
Recent studies show that individuals with hEDS experience:
Constipation at rates as high as 73% (compared to 16% in the general population)
Diarrhea in 47% of cases (vs. 9%)
Abdominal pain in 69%
Post-meal fullness in 34%
This is not a coincidence – and it’s not “just” IBS.
Why is the digestive system affected in EDS and HSD?
Because connective tissue is everywhere. And the GI tract, which depends on that tissue for both movement (motility) and structural support, is no exception.
When that connective tissue is too lax, too fragile, or improperly formed, it can interfere with digestion in several key ways:
Sluggish gut motility – leading to constipation, bloating, and even small intestinal bacterial overgrowth (SIBO) or small intestinal fungal overgrowth (SIFO)
Delayed gastric emptying – seen in some hEDS patients, causing nausea, fullness, and sometimes vomiting
Rectal or organ prolapse – where parts of the GI tract shift or drop, physically impeding stool passage
Increased sensitivity – due to abnormalities around the gut’s nerves, making digestion painful or unpredictable
Dysregulated autonomic nervous system (ANS) – especially in those with PoTS, which affects how the gut contracts and moves food
These issues often fall under the umbrella of functional gastrointestinal disorders (FGIDs) – such as irritable bowel syndrome (IBS) or functional dyspepsia – but for those with connective tissue disorders, the root causes are often structural and physiological, not simply “functional.”
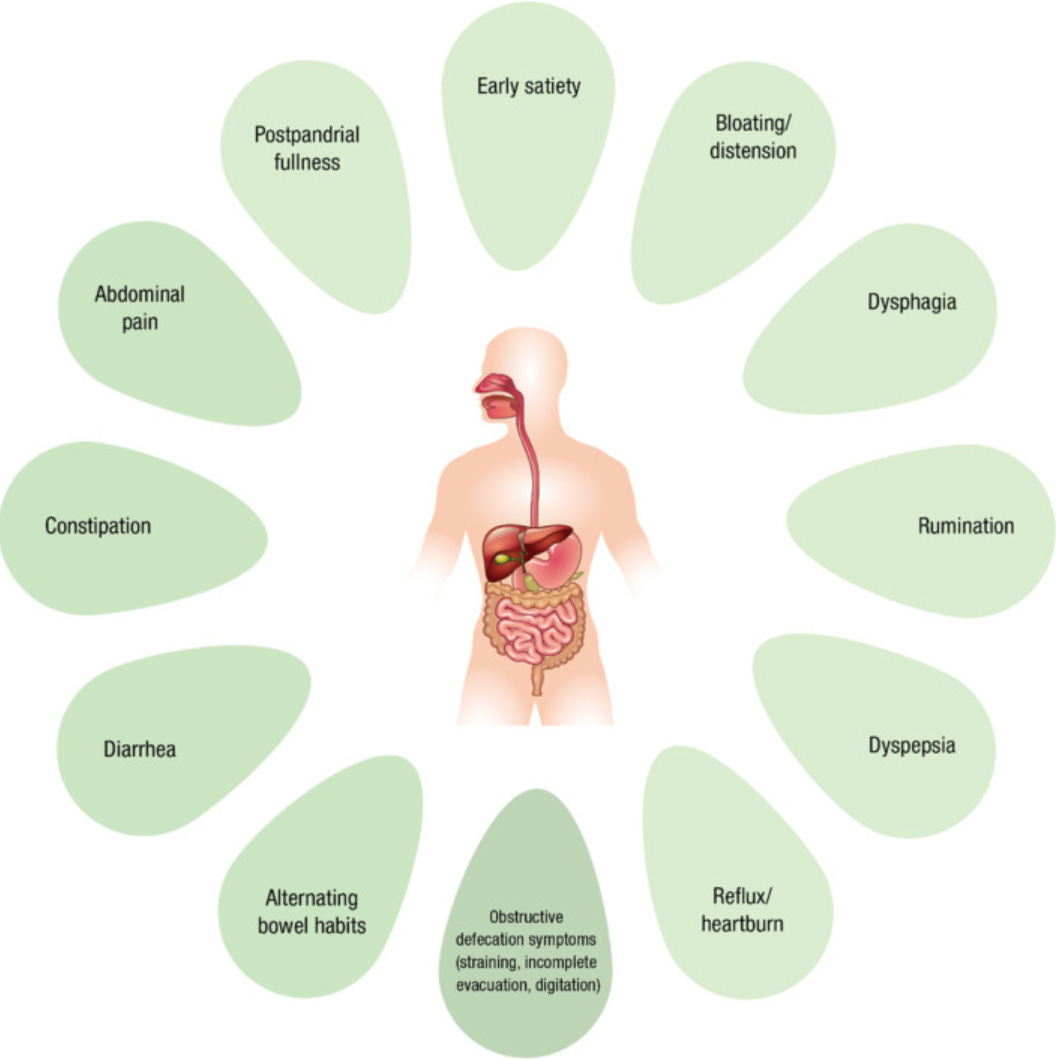
What about diarrhea? Isn’t EDS mostly linked to constipation?
Both can occur. Diarrhea may result from poor motility, autonomic dysfunction, SIBO, or even overlap with functional bowel disorders like IBS-D. The same patient can swing between both extremes – a phenomenon known as mixed bowel patterns – which can be particularly challenging to treat.
Other lesser-known GI manifestations in EDS-related disorders:
Heartburn and reflux (GERD) – sometimes related to small hiatal hernias, a loose lower esophageal sphincter, or dysmotility
Bloating – frequently reported but not well understood; SIBO, SIFO, and delayed transit are suspected contributors
Prolapse-related constipation – rectal, uterine, or bladder prolapse can interfere with bowel movements
Gastroparesis – rare but possible in severe delayed gastric emptying
GI bleeding or perforation – most common in vascular EDS (vEDS) and requires urgent attention
Poor surgical outcomes – especially in vEDS, where tissue fragility increases risk during and after GI surgery
So what can actually help?
There are no official, evidence-based GI guidelines for EDS and HSD – but we can still draw on clinical experience and emerging research to support symptom relief.
✅ Low FODMAP diets: Helpful for bloating and diarrhea, particularly in patients with overlapping IBS symptoms
✅ Prokinetics: Medications to stimulate gut movement in those with severe constipation or delayed gastric emptying
✅ Pelvic floor physical therapy: Especially for those with prolapse-related constipation or difficulty with evacuation
✅ Behavioral & psychological support: Cognitive behavioral therapy (CBT) and gut-directed hypnotherapy can improve symptom management, especially when anxiety or disordered eating play a role
✅ Specialist care: Many patients need a multidisciplinary approach – combining gastroenterology, pain management, physical therapy, and nutrition
What’s not recommended?
⚠️ Opioids – These slow the gut and worsen motility issues. They can lead to narcotic bowel syndrome and are best avoided for people with hEDS and HSD if at all possible.
⚠️ Dismissal – If a provider tells you that "everyone gets bloated" or "it's just IBS," it may be time for a second opinion.
What’s next?
More research. Despite the prevalence of GI issues in connective tissue disorders, we still don’t know:
Why some patients develop severe symptoms while others don’t
How connective tissue defects directly impair gut function
What role autonomic dysfunction plays in GI dysmotility
Which treatments are most effective in this population
Until we do, raising awareness, validating symptoms, and tailoring care plans to each patient remain our best tools.
GI symptoms in EDS and HSD are real, common, and often underrecognized.They deserve real answers – and better treatment options.
If you’re struggling with constipation, diarrhea, reflux, or bloating, you're not alone. And you're not making it up.
Here are some additional resources discussing constipation and diarrhea:
Episode 79 of Bendy Bodies: Gastrointestinal Problems in Hypermobile EDS
Gastrointestinal Involvement in the Ehlers-Danlos Syndromes (for Non-experts)
OUR SPONSOR
A huge shoutout to The Bendy Bodies Boutique for supporting today’s newsletter. It’s the perfect place to find something special for the zebra in your life. Explore our newest designs and remember you can personalize any item with your favorite store artwork. From clothing to home goods, there’s something for everyone.
Last Thursday, August 7th: Episode 157 with Dr. Pradeep Chopra
In the latest episode of Bendy Bodies, I am joined once again by pain specialist Dr. Pradeep Chopra for a guided tour through the GI tract. From teeth to intestines, we explore how conditions like EDS, HSD, POTS, and MCAS can wreak havoc on digestion and cause mysterious abdominal pain. We also shine a light on frequently missed diagnoses - like Eagle Syndrome, SIBO, and MALS - and share practical tips to help patients navigate these complex challenges. Don’t miss Part 1 of this two-part deep dive into GI issues in hypermobility!
This Thursday, August 14th: Season 5 Wrap with Dr. Linda Bluestein
As we close out Season 5 of the Bendy Bodies Podcast, I’m taking a moment to reflect on the conversations we’ve had, the feedback you’ve shared, and the incredible community we’ve built together. Thank you for being part of this journey - I can’t wait to show you what’s next.
DISCLAIMER
The information provided here is for educational purposes only and is not intended as a substitute for professional medical advice, diagnosis, or treatment. No physician-patient relationship is established by reviewing this material. Always consult your own healthcare provider or medical team before making any decisions about medications, supplements, or treatments. Dr. Bluestein is a licensed medical professional, but she is not your personal physician in this context and cannot provide individualized medical care, prescribe medications, order tests, or make referrals outside of a formal clinical relationship.
Some of the links shared are affiliate links. If you choose to purchase after clicking a link, I may receive a commission at no extra cost to you that helps support the mission of Bendy Bodies.
Well that’s all for this week; thank you so much for reading and supporting this newsletter. Talk to you soon, Bendy Buddies!
Yours in Health,
Dr. Bluestein







Very informative, thank you Doc.