Welcome to this week’s Bendy Bulletin! This week, we’re spotlighting an essential topic: why it’s critical to identify patients with hypermobility spectrum disorder (HSD) and hypermobile Ehlers-Danlos Syndrome (hEDS). Many healthcare professionals encounter these patients without realizing it, which can lead to missed diagnoses and ineffective treatments. In this newsletter, I’ll dive into why early recognition matters, how HSD/hEDS impacts multiple systems, and what you can do to improve outcomes for these patients. Whether you’re a healthcare professional or someone living with hypermobility, this is a conversation worth sharing!
If you’re an MD, NP, PA, or other healthcare professional, I feel confident that you are seeing patients with hypermobile joints - even if you don’t realize it at the time. Joint hypermobility is an underrecognized trait likely impacting 20% of adults and 34% of children. When it becomes symptomatic like with HSD or hEDS, there are significant implications for musculoskeletal health, pain management, and systemic care. As healthcare professionals, we should not let these opportunities pass us by. We can lessen symptom burden and improve quality of life.
Why You Should Care About HSD/hEDS
Patients with HSD/hEDS present with symptoms ranging from joint instability and musculoskeletal pain to systemic issues like fatigue, postural orthostatic tachycardia syndrome (POTS), gastrointestinal dysfunction, and poor tissue healing. Misdiagnosis or delayed recognition often leads to worse outcomes, as traditional interventions frequently fail or even exacerbate symptoms in hypermobile patients.
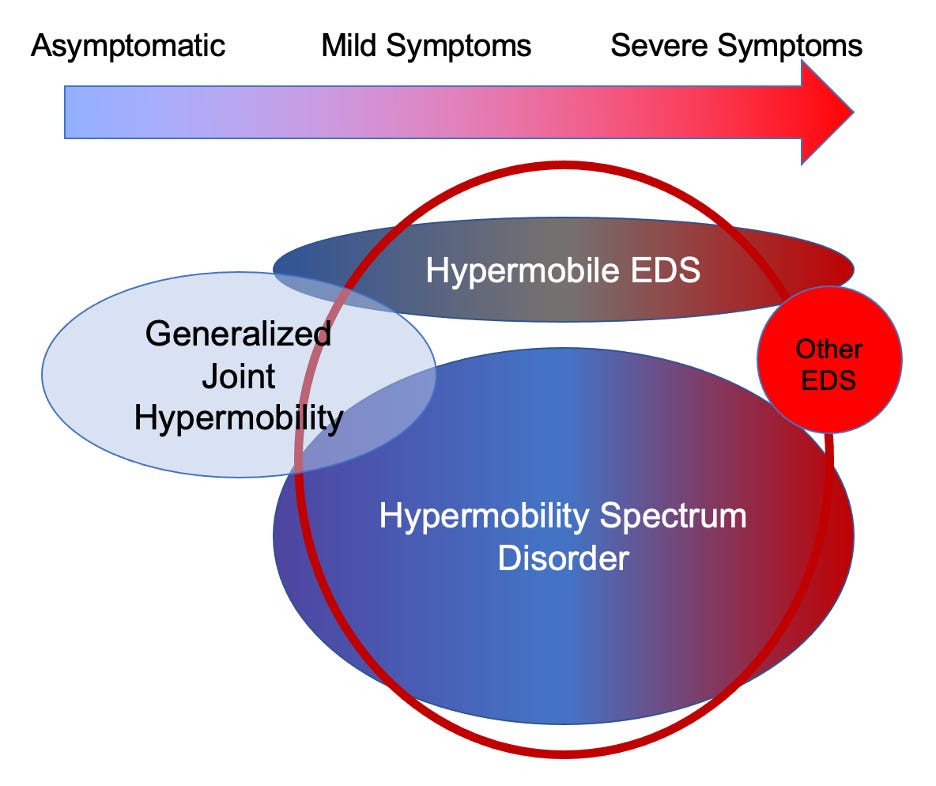
The Beighton score is a commonly used tool to assess for generalized joint hypermobility, but it has definite limitations. Core features of EDS besides hypermobile joints include stretchy skin and tissue weakness. Patients who don’t meet strict hEDS criteria or have another condition to explain their symptom may be diagnosed with HSD, which research shows can be just as debilitating. Both HSD and hEDS exist on a spectrum, requiring a nuanced approach to diagnosis and care. Recent research suggests that hEDS and HSD may not be distinctly different conditions after all.
"When You Can’t Connect the Issues, Think Connective Tissues"
Connective tissue and collagen are integral to nearly every part of the body. That means HSD/hEDS often presents with multisystem involvement. A patient complaining of ankle sprains, shoulder instability, or neck pain may also have fatigue, pseudo-seizures, or mast cell activation. Understanding these interconnected issues is essential for providing effective care.
How to Adapt Your Approach
Treating hypermobile patients requires caution and customization:
Evaluation: Learn how to assess generalized joint hypermobility and the diagnostic criteria for hEDS (watch for part 2 for more details).
Treat the Symptoms: Diversity amongst those with hEDS and HSD means that each patient must be treated according to whatever is most impacting their quality of life.
Titration: People with hEDS and HSD are often more sensitive to medications and require careful attention to dosages. Adverse reactions may be due to excipients (“inactive” ingredients) instead of to the medication itself.
Consider Other Disorders: Do not write everything off to hEDS/HSD, but remember that patients likely have other problems as well.
For movement professionals:
Start Low, Go Slow: These patients often don’t tolerate standard interventions well. Begin with lower-intensity movements focusing on proprioception and motor control, and progress gradually.
Tailor Manual Therapy: Use manual techniques judiciously, as fragile connective tissues are more prone to injury.
Educate on Joint Protection: Teaching body mechanics and joint protection strategies can prevent further damage and empower patients.
The Opportunity for Better Outcomes
Patients with HSD/hEDS are often labeled as "difficult" because their symptoms don’t fit the typical patterns, and they don’t respond well to standard protocols. By recognizing the “zebras” among the horses, we can improve outcomes and quality of life for these patients.
As healthcare professionals, it is our responsibility to adapt to the unique needs of hypermobile patients. Understanding their conditions - and the systemic issues that accompany them - can transform how we approach their care.
P.S. For additional information on hEDS and HSD, visit the Ehlers-Danlos Society website and listen to my podcast, Bendy Bodies. Let’s work together to ensure these patients get the care they deserve!
First, Do No Harm. Why You Should Identify Hypermobile Patients.
Read through the article by Dr Leslie Russek, DPT, that inspired today’s newsletter!
Curious on the role nutrition plays in managing hypermobility spectrum disorders (HSD) and Ehlers-Danlos Syndromes (EDS)? Check out our infographic that we made from the Bendy Bodies episode with Lorna Ryan.
LAST THURSDAY: Physical Therapist Wendy Wagner
We were thrilled to have physical therapist Wendy Wagner join the podcast, where she shared her expertise on managing hypermobility and connective tissue disorders through physical therapy. Wendy’s practical insights into tailoring treatment plans, improving body mechanics, and supporting patients with Ehlers-Danlos Syndromes offered valuable guidance for listeners looking to enhance their well-being and approach physical therapy with greater confidence.
THIS THURSDAY: Solo Episode
This week, it’s just me, Dr. Linda Bluestein, and I’m here to answer your burning questions about hypermobility, Ehlers-Danlos Syndromes (EDS), and everything in between! From navigating daily challenges to understanding complex medical concepts, I’ll be sharing insights and practical advice to help you better manage your health. Whether you’re curious about diagnosis, treatment options, or how to advocate for yourself, this solo episode is packed with information you won’t want to miss. Let’s dive into the topics you care most about and explore how to thrive with hypermobility.
Well that’s all for this week; thank you so much for reading and supporting this newsletter. Talk to you soon, Bendy Buddies!
Yours in Health,
Dr. Bluestein